How Fast Does Cancer Metastasize? A Reminder: The Body Often Shows These 4 Abnormalities When Cancer Spreads
Aunt Liu was a female worker at the village shoemaking factory, often busy with overtime work and irregular meals. After half a lifetime of hard work, she managed to raise two children and now has grandchildren, achieving a three-generation household.
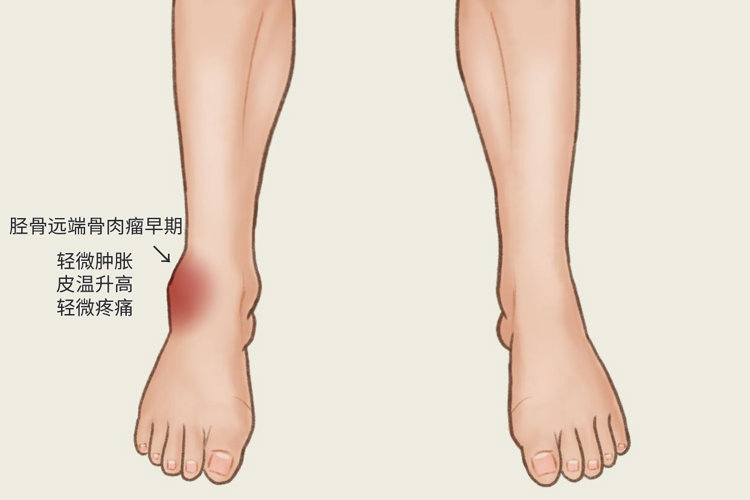
But just as autumn began, Aunt Liu noticed occasional pain in her ankle. At first, she thought it was rheumatism and didn’t pay much attention to it. But recently, even walking became difficult, so her son quickly took her to the hospital. After examination, a mass was found on her right kneecap, and she was diagnosed with osteosarcoma.
The doctor said: Fortunately, it was detected early, and the cancer was still in the early to middle stage, with no metastasis occurring. It could be completely cured through surgery. Aunt Liu felt relieved and was glad to hear the news.
1. Common Pathways of Cancer Metastasis
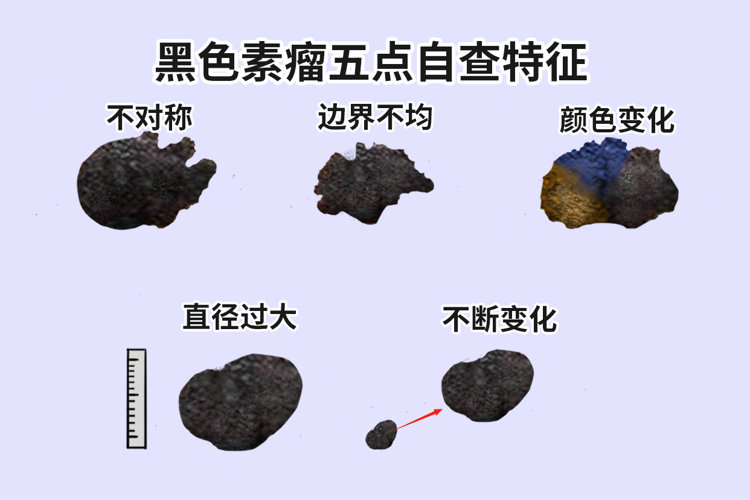
Cancer metastasis refers to the process where tumor cells break away from their original site, invade the circulatory system, migrate to other parts of the body, and continue to grow. However, not all cancers have the ability to metastasize, and this difference is particularly evident in skin cancer.
For example, basal cell skin cancer—a common non-melanoma skin cancer—hardly ever metastasizes; while the relatively rare skin cancer, melanoma, has a higher likelihood of metastasis.
Additionally, the speed of metastasis varies among different cancers—some spread rapidly, while others progress more slowly. The metastatic rate of cancer cells may differ depending on the type of cancer, but generally, the later the cancer is detected and treated, the greater the likelihood of metastasis.
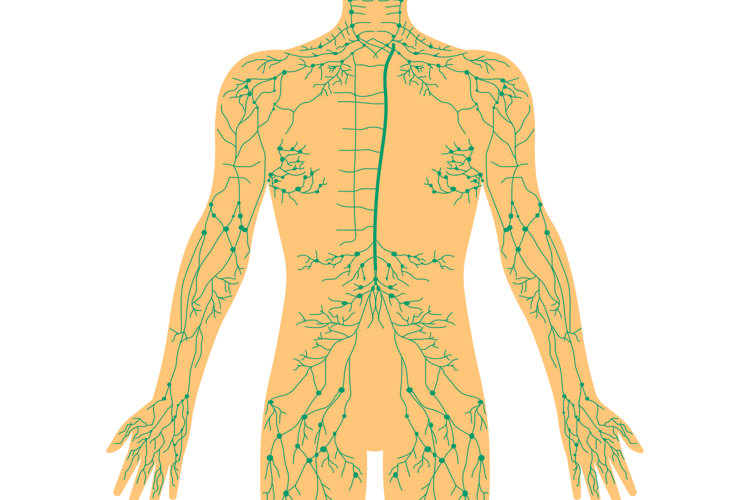
Cancer metastasis typically occurs through two main pathways: the lymphatic system and blood circulation. In contrast, benign tumors usually do not metastasize to distant sites.
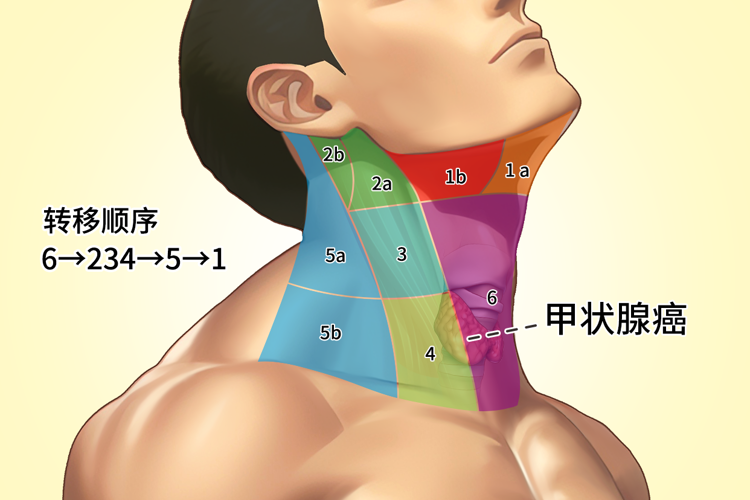
1. Lymph node metastasis
When cancer cells invade the lymphatic vessels, they may form detached emboli or directly proliferate within the lymphatic vessels, thereby forming continuous tumor masses.
Lymphatic metastasis occurs in the lymph nodes responsible for draining the tumor growth area, but if the lymph nodes are obstructed by a mass, retrograde spread may also occur, leading to the formation of metastatic lesions in unusual locations. Generally, the earlier lymph node metastasis appears, the more extensive the tumor spread becomes.
2. Hematogenous Metastasis
When tumor-containing lymph fluid enters the bloodstream, lymphatic metastasis evolves into hematogenous metastasis. Hematogenous metastasis typically occurs in advanced stages of cancer, but certain cancers such as lung cancer, breast cancer, kidney cancer, prostate cancer, and thyroid cancer may exhibit early hematogenous spread.

Cancer cells can move in the bloodstream either as individual cells or as clusters connected by fibrin. Clinically, some anticoagulants and chemotherapeutic drugs can reduce the risk of hematogenous metastasis; however, local compression or injury may increase the likelihood of hematogenous spread.
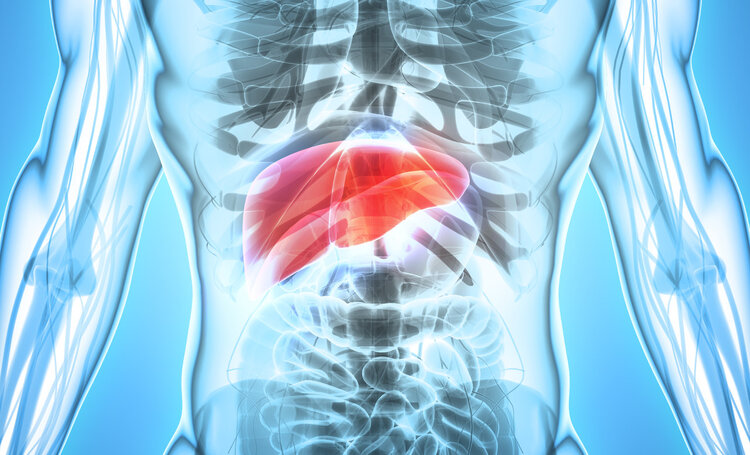
Currently, it has been discovered that in the human body, the liver is the most common site for metastasis, followed by the lungs, bone marrow, brain, and adrenal glands. In contrast, metastases to the spleen, muscles, and skin are relatively rare. This difference is related to the affinity of various tissues for metastatic cancer cells, though the exact mechanisms remain unclear.
Early detection and timely treatment are key to preventing cancer metastasis.
2. What symptoms appear before cancer cells metastasize or spread?
How to determine if a tumor may have metastasized? What are the common signs we should be aware of? Here are several symptoms that require attention:
1. Loss of appetite and weight loss
Tumor cells can release substances that affect appetite, leading to decreased desire to eat. If loss of appetite and weight loss occur despite stable treatment conditions, it could be a sign of tumor metastasis.

2. Unexplained lumps appearing on the body
While tumor growth inside the body often isn't visible to the naked eye, certain aggressive cancers can form lumps on the body's surface, such as lung cancer, stomach cancer, breast cancer, and head/neck malignancies. This may indicate tumor metastasis and warrants prompt examination at a specialized hospital or clinic.
3. Unexplained recurrent low-grade fever
Cancer patients in advanced stages often experience cancer-related fever (early-stage tumors may also occur, but with a lower incidence). If prolonged, recurrent low-grade fever appears and subsides on its own, with infection factors ruled out, vigilance is warranted for possible low-grade fever caused by tumor progression, as well as the risk of cancer recurrence or metastasis.

4. Worsening of pre-existing symptoms in the patient
After anti-tumor treatment, if a patient's existing symptoms suddenly worsen despite previous stabilization or improvement, caution should be exercised. This could indicate tumor recurrence or metastasis, necessitating further examination for disease assessment and prompt implementation of appropriate treatment measures.
5. Tumor marker levels rise
If early-stage cancer patients, after surgery, or advanced-stage patients during periods of treatment improvement and stability, observe a continuous rise in tumor markers, they should take it seriously even in the absence of obvious symptoms. They should promptly visit a specialized hospital or clinic for examination, as this is likely a signal of tumor recurrence or metastasis.

When noticing potential signs of tumor metastasis, seeking prompt medical attention is crucial to obtain accurate diagnosis and timely treatment, thereby maximizing quality of life and survival outcomes
3. How to Prevent Tumor Recurrence and Metastasis?
Preventing tumor recurrence and metastasis is a crucial and multifaceted challenge. Here are key measures that can help you receive optimal care and protection.
1. Standardized and comprehensive anti-tumor treatment
When undergoing treatment, patients must give their all to ensure they complete all recommended treatment courses, minimizing the risk of tumor recurrence and metastasis. For those who find the treatment intolerable, close collaboration with doctors is essential to adjust the treatment plan, rather than self-terminating therapy or altering medication dosages without authorization.

Improve physical constitution and build a robust defense system
1. Break bad habits: For example, lung cancer patients should quit smoking, and liver cancer patients should actively treat hepatitis while avoiding alcohol abuse. Additionally, avoiding moldy foods and reducing intake of pickled and fried foods can also help prevent tumor recurrence and metastasis.

② Balanced nutrition: Since cancer is a wasting disease and treatments (such as surgery and chemotherapy) can compromise a patient's nutritional status and immune function, prioritizing balanced nutrition is crucial. Cancer patients are advised to consume plenty of vegetables, fruits, and foods rich in vitamins and minerals, while also increasing intake of high-quality proteins to meet the body's nutritional and energy needs.
3. Regular exercise: Moderate physical activity can enhance the body's immune function and help reduce the risk of tumor recurrence. Patients should choose suitable exercise methods based on their specific physical conditions—such as Tai Chi, jogging, or yoga—to maintain health and vitality.

3. Maintain a cheerful mood and seek appropriate psychological counseling when needed.
Cancer patients are often prone to anxiety and despair, and prolonged negative emotions can impair immune system function, increasing the risk of tumor recurrence and metastasis. Therefore, maintaining an optimistic mindset, along with appropriate psychological counseling and support, is crucial for preventing tumor recurrence and metastasis.

4. Regular check-ups without relaxation
Patients should undergo regular follow-up examinations to detect any possible signs of recurrence or metastasis early. They should closely monitor their physical condition, such as paying attention to any newly developed lumps, irregular bleeding, persistent coughing, or other abnormal symptoms, and report them to a doctor promptly.
The frequency of follow-up examinations should be determined based on the patient's specific condition and the doctor's recommendation. The commonly suggested follow-up plan is: within 1-2 years post-surgery, a comprehensive check-up every 3 months; 2-3 years post-surgery, a comprehensive check-up every 6 months; and more than 3 years post-surgery, a comprehensive check-up every 6-12 months.

Summary: Generally, the likelihood of cancer cells spreading in the early and middle stages is relatively low, so the best way to treat cancer is early detection and early intervention. It’s crucial to pay attention to bodily changes, undergo regular check-ups, and seek medical attention promptly for unexplained illnesses.