"Fatty Liver Disease" Rises as China's Top Liver Condition, 125 Targeted Drugs in Accelerated R&D
Non-alcoholic fatty liver disease (abbreviated as NAFLD, also known as metabolic dysfunction-associated steatotic liver disease) has grown rapidly and inadvertently surpassed hepatitis B to become China's most prevalent chronic liver condition.
Data from The Lancet shows that the number of people with fatty liver disease in China has exceeded 200 million. Among them, over 120 million suffer from non-alcoholic fatty liver disease. Middle-aged men over 40 are one of the primary high-risk groups for this condition.
Despite the large number of fatty liver patients, most men do not take this condition seriously.
Worldly-wise middle-aged individuals believe that compared to ego-shattering sexual dysfunction, life-threatening heart attacks, or debilitating strokes, mild fatty liver disease hardly warrants discussion—it presents no symptoms, causes no pain, and progresses slowly, making it seemingly unworthy of concern.
What they fail to realize is that fatty liver disease is a "frog-in-boiling-water" condition. Years of accumulated fatty liver can still lead to fatty liver hepatitis, liver fibrosis, cirrhosis, and even progress to liver cancer. It maintains intricate and special connections with the occurrence of malignant tumors and cardiovascular diseases.
Is fatty liver detected during a physical exam becoming "cancer" three years later?
"Me? Liver cancer—are you sure there's no mistake?" In the largest liver disease center in the provincial capital, 40-year-old Ou Hao (pseudonym) trembled as he held the test report, his face full of disbelief, repeatedly asking the doctor for confirmation.
"It is indeed liver cancer, and the situation isn't very good (mid-to-late stage). You need treatment as soon as possible." The bespectacled doctor in his fifties carefully reviewed Ou Hao's medical history and past physical exam reports, finding no evidence of hepatitis B infection but noting a fatty liver diagnosis three years earlier. This, he suspected, might have been the hidden danger that led to the current situation.
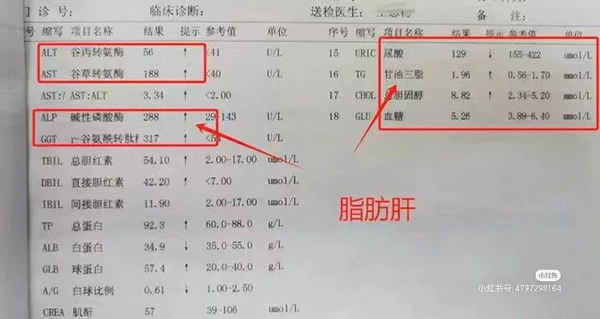
◎ Be alert to fatty liver if these abnormal indicators appear on your test results. / Image: Xiaohongshu
A normal liver contains a small amount of fat, typically accounting for 3%-5% of the liver's weight. When the fat content exceeds 5% or when histological examination shows fat deposition in over 5% of hepatocytes, it can be diagnosed as fatty liver disease. Based on etiology, fatty liver is further classified into alcoholic fatty liver disease and non-alcoholic fatty liver disease.
When the doctor inquired about his daily eating habits, Ou Hao said he had been habitually replacing water with sugary drinks since high school. After starting work, he consumed milk tea and coffee daily. Strangely, his physique remained largely unchanged—standing 170 cm tall, his weight consistently stayed around 65 kg, leading colleagues to envy him with comments like, "You're so genetically lucky—you never gain weight no matter what you eat."
"Because I never really got fat, I didn't take the fatty liver diagnosis seriously at the time," Ou Hao admitted. Upon receiving his medical report, he noticed the term "fatty liver" and asked the examiner about it. He was told it was mild fatty liver—reversible with dietary adjustments.
"My health has generally been good, and this condition causes no noticeable discomfort, so I never followed up with doctors. When work got busy, I quickly forgot about having fatty liver." Over the past three years, Ou Hao maintained his original lifestyle—staying up late when necessary, drinking alcohol freely, and regularly consuming high-calorie foods like fried chicken and kebabs.
Recent studies have shown that the proportion of liver cancer patients with a history of fatty liver (steatohepatitis) is gradually increasing. In the United States, the annual increase rate of liver cancer among non-alcoholic fatty liver disease (NAFLD) patients is about 9%, and their survival period is shorter than that of hepatitis B or C patients.
A recent study published in a sub-journal of the *Journal of the American Medical Association* (*JAMA Network Open*), conducted by researchers from Beijing Shijitan Hospital affiliated with Capital Medical University and other institutions in China, analyzed long-term follow-up and comparative data of 63,000 individuals. The findings revealed that developing fatty liver before the age of 45 increases the overall probability of cancer in later years by 50%, with risks of digestive tract cancers, liver cancer, lung cancer, and colorectal cancer at least doubling.
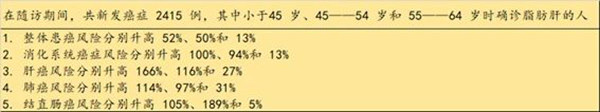
◎ Study of 60,000 Chinese: Fatty liver before age 45 increases cancer risk in later years./ Illustration by Deep Breath.
However, the vast majority of fatty liver cases show no obvious symptoms, so whether it's mild, moderate or severe fatty liver, what deserves more attention is the presence of inflammation and fibrosis.
If there is inflammation and fibrosis, it is classified as progressive fatty liver disease, which increases the risk of developing cirrhosis and liver cancer. Particularly for those over 40 years old who are diagnosed with fatty liver during physical examinations, further consultation should be sought at specialized departments such as hepatology, gastroenterology, or endocrinology.
The seemingly ordinary fatty liver has truly become a new challenge.
Fatty liver most commonly occurs in people with obesity, poor dietary habits, lack of sleep, and insufficient physical activity. The majority of fatty liver patients do not have excessive alcohol consumption.
Statistics show that the prevalence of non-alcoholic fatty liver disease (NAFLD) in China is as high as 15%, accounting for 49.3% of chronic liver diseases. Among obese patients, 60% to 90% have non-alcoholic fatty liver.
Current understanding suggests that a diet high in fat and calories, a sedentary lifestyle, insulin resistance, metabolic syndrome and its components (obesity, hypertension, dyslipidemia, and type 2 diabetes) can all lead to non-alcoholic fatty liver disease.
Obesity is a significant factor in the development of fatty liver disease, but not the only one. Heavy alcohol consumption and diets high in sugar, fat, and carbohydrates increase the risk of fatty liver, yet solely eating plant-based foods or extreme dieting may not necessarily benefit liver health.

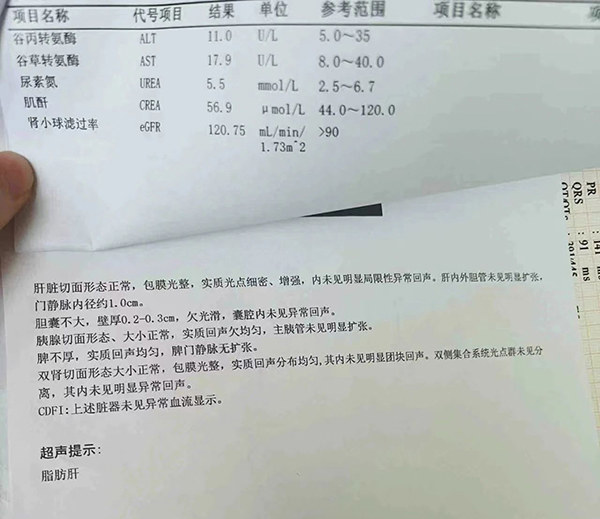
◎ Be cautious of "starving" yourself into fatty liver disease by excessive dieting. / Photo: Sharp Image Visual
"Doctor, how could I possibly have fatty liver disease?" Dalu (a pseudonym), a vegetarian weighing only 105 pounds, was completely stunned when he received his physical examination results. Two years ago when he was overweight, he began a no-carb diet to lose weight - eliminating staple foods like rice and noodles, eating only low-fat seafood for meat, and boiling all vegetables. Within six months, he had lost 40 pounds.
Unexpectedly, during this March's physical exam, Dalu received a health warning for "moderate fatty liver disease." The doctor advised him to adjust his dietary structure, increase exercise, actively improve metabolic conditions, and undergo targeted drug treatment.
Too extreme is as bad as not enough. Improper dietary control - such as excessive dieting, long-term vegetarianism, or insufficient protein intake - can lead to apolipoprotein deficiency and lipid metabolism disorders, actually worsening hepatic fat accumulation. Doctors refer to this as "starvation-induced fatty liver." This represents a key difference between fatty liver and other metabolic diseases.
Additionally, common causes of fatty liver in lean individuals include phosphorus poisoning, drug-induced liver damage, hyperthyroidism or hypothyroidism, severe anemia, and chronic cardiopulmonary insufficiency.
Professor Chen Yongpeng, Chief Physician of the Infectious Diseases Department at Nanfang Hospital of Southern Medical University, pointed out that fatty liver disease has become a new challenge following hepatitis B and C, with a continuously growing number of affected individuals and a clear trend toward younger patients. Its causes are numerous, and people of any body type—whether overweight or lean—can develop fatty liver disease.
What is particularly concerning is that among individuals with non-alcoholic fatty liver disease who also have metabolic syndrome or type 2 diabetes, the detection rate of non-alcoholic steatohepatitis (NASH) is very high. This form of hepatitis has a 10–15-year cirrhosis incidence rate as high as 15–25%, with 16% of cirrhotic patients progressing to liver cancer within 5 years.
The harm of fatty liver disease goes far beyond the liver itself. It affects multiple systems throughout the body, including disrupting lipid metabolism, elevating blood sugar and blood pressure, and accelerating atherosclerosis. This significantly increases the risk of cardiovascular and cerebrovascular events, making individuals more susceptible to severe life-threatening or disabling conditions such as cerebral infarction, cerebral hemorrhage, and myocardial infarction.
If fatty liver disease is diagnosed, timely intervention or treatment can reduce the risk of many serious conditions in the future. "However, unlike hepatitis B and C, which have specific medications for treatment and long-term disease control, there is currently no effective drug for fatty liver disease," said Chen Yongpeng. He explained that drugs are still in the clinical research stage, and doctors have limited options, only being able to advise patients to undergo regular check-ups to monitor the condition.
No effective drugs for steatohepatitis? 125 new drugs in development in China
The lack of medications that can provide immediate relief is another major reason why many people do nothing after being diagnosed with fatty liver disease.
On April 28th, I was diagnosed with fatty liver disease. The doctor advised me to exercise more, eat less greasy food, and maintain a regular sleep schedule. / Image: Xiaohongshu @EatAnApple
Doing something feels more reassuring than doing nothing at all. Some fatty liver patients turn to lipid-lowering health supplements or traditional Chinese dietary therapies for relief. While these may offer some benefits for mild fatty liver disease, they are completely unrealistic and unreliable for reversing advanced stages accompanied by inflammation and fibrosis.
The reality is that current treatment for simple fatty liver primarily relies on lifestyle modifications, including dietary changes, exercise therapy, and psychological adjustments.
For fatty liver progressing to non-alcoholic steatohepatitis (NASH), beyond lifestyle improvements and managing underlying conditions, anti-inflammatory and liver-protective medications are often used. However, these treatments show limited effectiveness, and there remains a lack of widely proven drugs for liver injury.
Statistics show that in 2020, there were 350 million global cases of non-alcoholic steatohepatitis, expected to rise to 410 million by 2025 and reach 480 million by 2030.
The situation in China is even more severe, with a prevalence rate of non-alcoholic fatty liver disease (NAFLD) diagnosed by B-ultrasound in the general adult population reaching 31%, surpassing the global incidence rate of 25.2%. By 2025, it is projected that new cases of non-alcoholic steatohepatitis (NASH) in China will increase to 2 million, twice the number of new cases of non-small cell lung cancer.

Issues such as hepatitis and fibrosis caused by fatty liver urgently require effective medication. / Image: Panoramic Vision
The massive patient population signifies enormous market demand. Industry analysts predict: following the explosion of kinase inhibitors (TKI), the crowding of PD-1 drugs, and the battles in ADC and CAR-T therapies, the next billion-dollar pharmaceutical market will likely be drugs for nonalcoholic steatohepatitis (NASH).
Just last month, the U.S. Food and Drug Administration (FDA) granted accelerated approval for Resmetirom, developed by Madrigal Pharmaceuticals, for treating nonalcoholic steatohepatitis (NASH) patients with liver fibrosis. This marks the first innovative drug approved by FDA specifically for NASH treatment.
According to data from the Patsnap Global New Drug Intelligence Database, there are currently 445 drugs worldwide under development targeting non-alcoholic steatohepatitis (NASH), including the approved Resmetirom. China has 125 related drugs in development. Domestic pharmaceutical companies such as Ascletis, Innovent Biologics, Livzon Pharmaceutical, Chia Tai Tianqing, and Haisco are actively engaged in NASH drug development through independent research or licensed introductions.
It is believed that in the near future, patients with non-alcoholic steatohepatitis in our country will also have access to specialized medications.
For individuals currently with fatty liver disease, the achievable priority is self-health management: weight loss for obesity, blood sugar control to prevent diabetes, and regular monitoring through ultrasound examinations, liver function tests, complete blood counts, liver elastography, lipid profiles, and blood glucose tests to track liver health and potential metabolic disorders.