Common Causes of Male Infertility: Varicocele – The "Silent Killer" in the Scrotum
In the outpatient clinic, many young men come for consultation after prolonged unsuccessful attempts at conception. When their semen is examined, decreased sperm count and motility are often detected. Further color Doppler ultrasound examinations frequently reveal that the culprit is varicocele. This seemingly minor and asymptomatic condition is referred to as the "silent killer in the scrotum" because its damage to male fertility is often long-term and insidious.
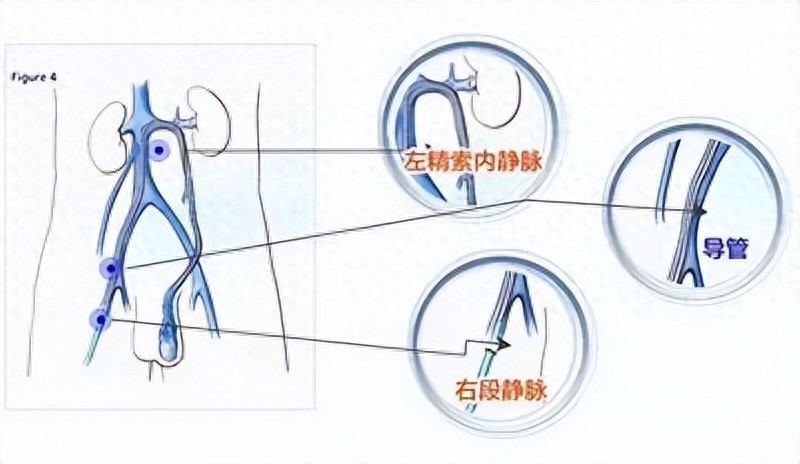
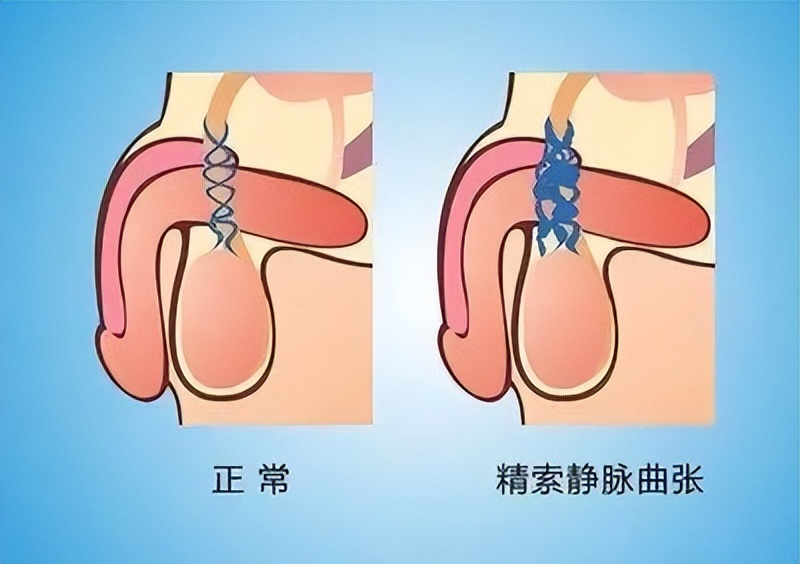
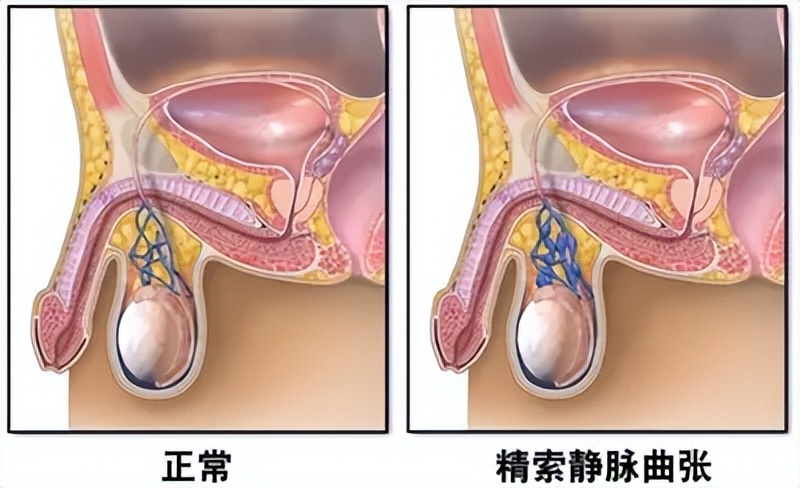
The spermatic cord veins are a group of blood vessels surrounding the testicles, responsible for returning venous blood from the testes back to systemic circulation. If the valves in these veins malfunction, blood may reflux and accumulate, causing vascular dilation and tortuosity—this condition is known as varicocele. It's essentially "varicose veins" on the testicles, similar in mechanism though occurring in a different location.
01 What is Varicocele?
Varicocele primarily harms fertility through two mechanisms: first, it raises testicular temperature, disrupting the normal spermatogenic environment; second, blood stasis generates large amounts of metabolic waste and free radicals that are toxic to sperm. Over time, this leads to decreased sperm count, reduced motility, and increased abnormal forms. Studies show approximately 40% of infertile men have varicocele.
02 Why does it cause infertility?
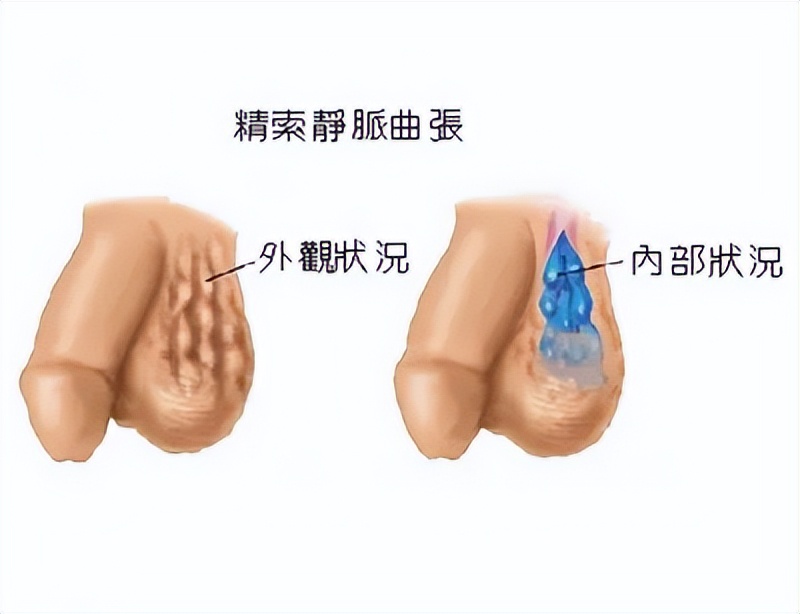
Some patients experience a sensation of scrotal heaviness, particularly aggravated by standing or prolonged walking, which often alleviates when lying down to rest. Others may feel dull testicular pain or a cold sensation, and in severe cases, one might even palpate a cluster of "worm-like" varicose veins in the scrotum. However, many show almost no noticeable symptoms and only discover the condition when investigating infertility issues—precisely why it's termed the "silent killer."
03 What are the typical symptoms?
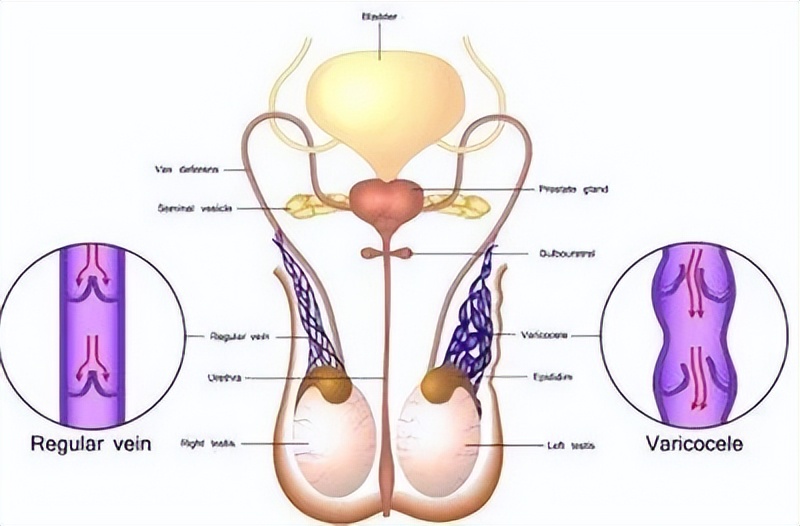
The most commonly used diagnostic tool is scrotal color Doppler ultrasound, which visually demonstrates the extent of venous dilation and reflux. Clinically, varicoceles are classified as mild, moderate, or severe based on the diameter of the dilated veins and the degree of reflux. Patients with mild cases and no fertility concerns may simply be monitored, while those with abnormal semen quality or infertility symptoms require further intervention.
04 How is it diagnosed?
Currently, the most effective treatment is microscopic varicocelectomy. The surgery blocks refluxing veins, restoring normal testicular blood circulation to improve both testicular function and sperm quality. Studies show that most patients experience significant improvement in semen parameters post-surgery, with some couples achieving natural conception. For those who don’t fully recover, assisted reproductive technologies can be utilized to enhance pregnancy chances.
05 What are the treatment options?
06 Lifestyle adjustments are also necessary
Even after surgery, daily care is equally important. Patients should avoid prolonged standing or sitting, reduce heavy physical labor, keep the scrotum cool and well-ventilated, and prevent excessive staying up late and mental stress. Additionally, quitting smoking, limiting alcohol intake, maintaining a balanced diet, and exercising more all help improve the spermatogenic environment.
Varicocele may seem like a "minor issue," but it can be a major hidden threat leading to infertility. Many young men feel too embarrassed to seek medical attention, often delaying diagnosis until years of unsuccessful attempts at conception after marriage. My advice is: if pregnancy attempts fail after over one year, men must undergo comprehensive examinations, with particular attention to varicocele screening. Only through early detection and timely treatment can fertility potential be properly safeguarded.