What Cancers Are Prone to Liver Metastasis? What to Do After Liver Metastasis?
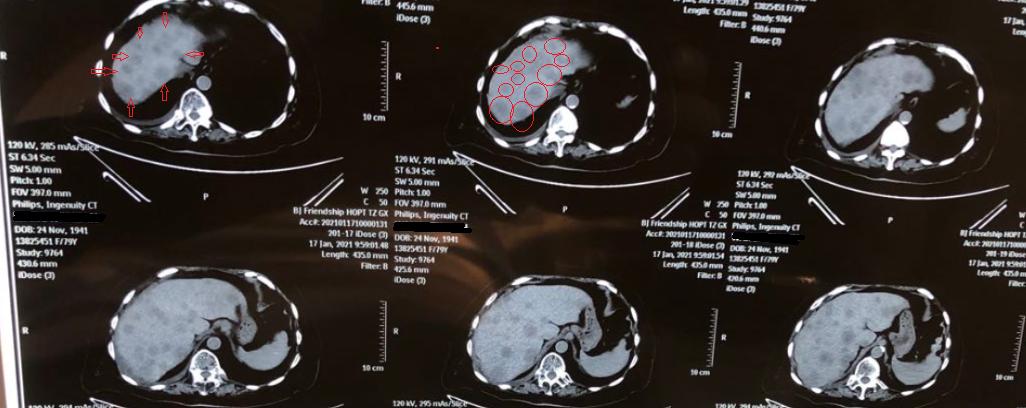
Recently, another patient with liver metastasis of cancer came to the outpatient clinic. Looking at the CT scan, my heart sank. The primary lesion itself wasn’t too problematic, but there were too many liver metastases. Just in one cross-section of the CT scan, more than ten visible metastatic foci could be seen.
The liver is a vital organ in the human body, performing many important functions such as metabolism, detoxification, and digestion. Traditional Chinese Medicine holds that the liver stores blood and governs free flow, managing the storage and regulation of blood. When cancer metastasizes to the liver, it severely impairs liver function, leading to changes in multiple systems of the body, including metabolism, digestion, and blood circulation. This often poses a serious threat to life in a short period of time.
I. Which Cancers Are Prone to Liver Metastasis?

The liver receives dual blood supply from the hepatic artery and portal vein, resulting in exceptionally rich blood flow. This provides a favorable environment for hematogenously spreading cancer cells to grow. Therefore, tumors from any site can potentially metastasize to the liver via the bloodstream. However, clinically, metastases from the lungs, breast, colon, pancreas, and stomach are more common, with gastrointestinal tract tumors exhibiting a relatively high incidence of liver metastasis.
Gallbladder cancer often metastasizes to the liver via the lymphatic system; breast cancer and lung cancer can also metastasize retrogradely to the liver through lymphatics, though this is less common clinically. Tumors from organs adjacent to the liver can directly invade and spread to the liver, such as tumors of the stomach, transverse colon, gallbladder, pancreas, kidney, and adrenal glands.
II. How Are Liver Metastases Detected?

Late-stage detection is very easy, as seen with the patient mentioned at the beginning of the article, where both the symptoms and the findings on the CT scan are quite obvious. However, in the early stages, when the lesions are small, diagnosis is relatively difficult.
Since the liver parenchyma lacks sensory nerves, while the liver capsule is rich in sensory nerve fibers, noticeable discomfort is often absent in the early stages of liver disease. Only when the entire liver enlarges, causing overstretching and increased tension of the liver capsule, does pain in the liver region occur. Therefore, in the early stages, various diagnostic methods must be combined for analysis.
1. Liver Function
The most common abnormalities in liver disease involve changes in transaminase and bilirubin levels. Abnormalities in tests such as alkaline phosphatase, lactate dehydrogenase, and albumin are also of significance.
2. Tumor Markers
Elevated carcinoembryonic antigen (CEA) is most commonly seen in gastrointestinal cancers, which are also malignancies prone to liver metastasis. This has certain significance for the diagnosis of liver metastasis.
Changes in tumor markers are also important indicators for evaluating treatment efficacy and progression after therapy for malignant tumors. An increase in tumor markers after treatment completion may suggest possible liver metastasis.
3. Ultrasound
B-ultrasound is the most common examination method for liver diseases, capable of detecting lesions as small as 1-2 cm. It offers the advantages of low cost, high accuracy, and ease of accessibility.
4. CT
CT is a relatively precise examination method for diagnosing liver metastatic tumors, with higher sensitivity than ultrasound. However, it may miss tiny lesions.
5. MRI
MRI, or magnetic resonance imaging, also commonly known as nuclear magnetic resonance, is a highly sensitive examination method for diagnosing liver metastasis, capable of detecting lesions smaller than 1 cm.
6. Other
Including PET-CT, liver biopsy, laparoscopic exploration, etc., these are high-accuracy examination methods but come with disadvantages such as high cost, significant damage, and numerous restrictions, and are not used as routine tests.
III.

The treatment for liver metastases differs from that for primary liver cancer, as the biological activity of liver metastases is the same as that of the primary lesion. Therefore, when selecting a treatment plan, the pathological results of the primary lesion must be considered.
1. Surgery
Surgical resection can be performed in the early stages of metastasis, achieving good outcomes and enabling long-term survival; if the metastases are large or numerous, surgery is generally not recommended.
2. Chemotherapy
The chemotherapy regimen for liver metastases is the same as that for the primary tumor, which can reduce tumor size and prolong life. Systemic chemotherapy has a killing effect on the primary tumor, liver metastases, and other detected or undetected lesions, but it has significant side effects that are often intolerable for advanced-stage patients.
3. Interventional Therapy
Liver interventional therapy is a local treatment method involving catheter insertion through the femoral artery to inject drugs or embolic agents into the hepatic artery, which is a commonly used treatment for liver tumors.
Interventional therapy typically employs chemotherapeutic agents, which can more directly target and destroy liver metastatic tumors, resulting in significantly fewer side effects compared to systemic chemotherapy.
Embolic agents can block tumor vessels, cut off blood supply to tumors, thereby inhibiting tumor growth. Through injection of embolic agents, the effect of "starving" the tumor can be achieved.
4. Traditional Chinese Medicine Treatment
Traditional Chinese medicine treatment can adopt different therapeutic approaches based on varying body constitutions and conditions, effectively alleviating symptoms and extending survival.
However, traditional Chinese medicine alone cannot completely alter the prognosis; a combination of Chinese and Western medicine is needed to achieve better outcomes.