The Future of Cancer Treatment: How Effective is Immunotherapy Combined with Traditional Chinese Medicine?
In August 2015, former U.S. President Jimmy Carter was diagnosed with melanoma, which had already metastasized to the brain and liver.
According to the traditional staging method, melanoma can be divided into five stages: 0–IV. Stage 0 refers to carcinoma in situ, Stages I and II are localized tumors, Stage III involves lymph node metastasis, and Stage IV, which is President Carter’s stage, indicates distant metastasis.

We all know that the prognosis of tumor treatment is significantly related to staging; the later the stage, the worse the prognosis, with stage IV being the stage with the poorest prognosis.
However, in December 2015, Carter announced that the tumor in his brain had disappeared. A follow-up examination in February 2016 found no melanoma in any part of his body.
To achieve such results in just half a year—what exactly did he do?
The miraculous PD-1.
Former U.S. President Carter, after his diagnosis, received assistance from numerous top experts across the United States, who devised the most advanced treatment plan available at the time. This involved first surgically removing the liver metastases, followed by radiotherapy to control the brain tumor, and finally taking immunotherapy drugs.
Carter was prescribed the PD-1 inhibitor pembrolizumab, commonly known as Keytruda, which was the first PD-1 inhibitor approved and launched in 2014.

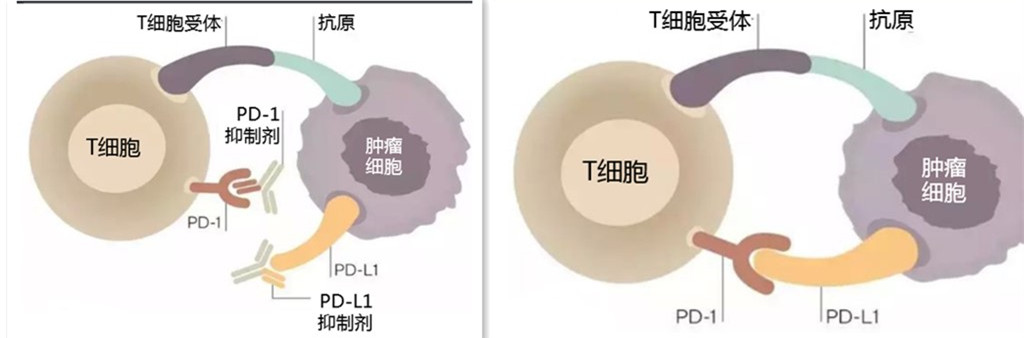
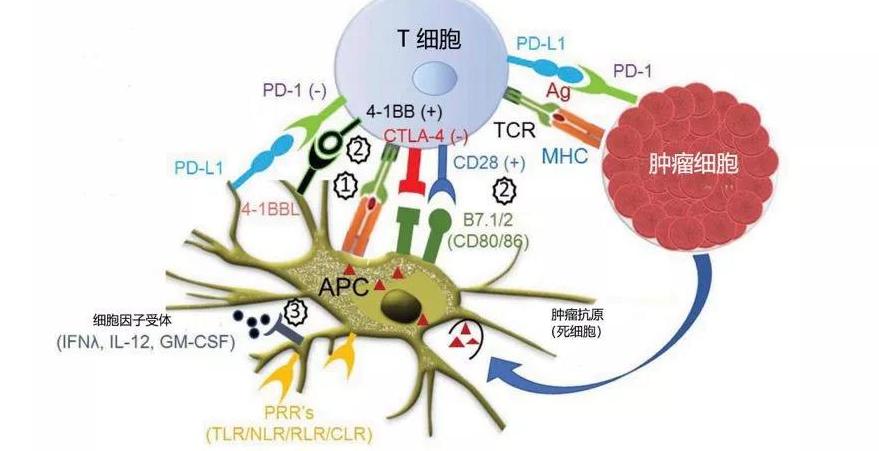
PD-1 stands for programmed cell death protein 1, an important immune checkpoint molecule that helps prevent autoimmune diseases but can also inhibit the immune system from killing cancer cells, allowing them to grow uncontrollably. PD-1 inhibitors work by blocking PD-1, thereby activating the immune system to target and eliminate tumors in the body.
Carter was 91 years old when diagnosed with melanoma and is now 96. On August 5, 2020, he even sent a congratulatory letter to the U.S.-China People-to-People Diplomacy Video Dialogue, demonstrating his continued dedication to improving U.S.-China relations.
Since then, PD-1 has gained immense popularity, and Carter became the "living advertisement" for PD-1 therapy.
Research on Immunotherapy
Currently, the most extensively studied aspects of tumor immunotherapy are PD-1 and PD-L1. PD-L1 is a counter-receptor; tumor cells express PD-L1 to bind with PD-1, thereby evading the immune system's attack.
PD-1 inhibitors and PD-L1 inhibitors work by blocking these pathways, enabling the immune system to correctly identify cancer cells and achieve the goal of eliminating tumors through the body's own immune response.
In recent years, several PD-1 and PD-L1 monoclonal antibodies have been approved for marketing and widely used in clinical practice. Examples include PD-1 inhibitors such as nivolumab, pembrolizumab, and tislelizumab, as well as PD-L1 inhibitors like atezolizumab, durvalumab, and avelumab.
In addition to treating melanoma, PD-1 and PD-L1 inhibitors can also be used in the treatment of various other malignancies, including non-small cell lung cancer, renal cell carcinoma, bladder cancer, Hodgkin lymphoma, urothelial carcinoma, and gastric cancer.
Current animal studies indicate that PD-1 inhibitors may also play a role in the treatment of AIDS and Alzheimer’s disease.
Drawbacks of immunotherapy
First, Effectiveness
Is immunotherapy so miraculous that it can consistently achieve good results in practical applications?
The answer is no. According to statistics, the response rate of PD-1 inhibitors in unselected solid tumor patients is only 10% to 30%, while the response rate is above 60% only in classical Hodgkin lymphoma.
Actually, when performing immunohistochemistry, we can test for PD-L1 expression—the higher the PD-L1 expression, the more effective PD-1 inhibitors tend to be.
In response to this situation, several solutions have been proposed, including combination therapy with other inhibitors such as CTLA-4 antibodies, as well as combined approaches with chemotherapy, radiotherapy, targeted therapy, and traditional Chinese medicine. These strategies can enhance effectiveness and enable patients to achieve longer-term survival.
II. Side Effects
Side effects are an unavoidable issue in tumor treatment. Common side effects of immunotherapy include nausea, vomiting, fatigue, constipation, fever, rash, pneumonia, and liver and kidney damage. Different drugs also have distinct profiles; for example, nivolumab commonly causes rash, while atezolizumab is frequently associated with nausea, fatigue, and urinary tract infections.
III. Drug Resistance
Generally speaking, patients who respond effectively to tumor immunotherapy can maintain long-term efficacy, but some patients may still experience recurrence, which is caused by drug resistance. Once drug resistance occurs, treatment with the medication will no longer provide benefits.
IV. Price
Immunotherapy, targeted therapy, and traditional Chinese medicine are regarded as the "lifelines" for cancer patients, serving as the last resort for many with malignant tumors. Targeted drugs have gradually been included in the medical insurance list, and most traditional Chinese herbal medicines have long been covered under medical insurance reimbursement. However, among immunotherapy drugs, very few are covered by medical insurance, and their high prices deter many.
At the end of 2019, the PD-1 monoclonal antibody drug, Dabasu (sintilimab injection), was officially included in the medical insurance coverage through price negotiations, becoming the first PD-1 monoclonal antibody drug to be listed in the national medical insurance directory.
In the future, it is believed that more PD-1/PD-L1 drugs will be included in the national healthcare coverage.
The Difference Between Traditional Chinese Medicine for Boosting Immunity and Immunotherapy
Immunotherapy aims to eliminate tumors by modulating the immune system, which may sound similar to traditional Chinese medicine at first glance. Traditional Chinese medicine can suppress tumors by enhancing overall immunity. However, given the fundamental differences in theories between Chinese and Western medicine, they should not be simplistically equated.
1. Traditional Chinese Medicine and Immunity Enhancement
Many components in traditional Chinese medicine have immunomodulatory effects, including organic acids, polysaccharides, glycosides, alkaloids, volatile oils, and more. For instance, ginseng polysaccharides can promote hematopoietic function recovery and enhance macrophage phagocytic activity; matrine has antimicrobial and antiviral effects; astragalosides regulate the functions of immune cells such as T cells and B cells; and saikosaponins inhibit influenza viruses, increase macrophage activity, and also promote the growth and function of splenocytes.
The diverse components of traditional Chinese medicine exhibit multifaceted effects, particularly in herbal decoctions, which place greater emphasis on enhancing overall immunity.

2. Tumor Immunotherapy and Immune Function
Tumor immunotherapy targets a single pathway; currently commonly used PD-1 drugs such as pembrolizumab and nivolumab, as well as PD-L1 drugs like atezolizumab and durvalumab, all target the PD-1/PD-L1 pathway and have almost no effect on other immune functions.
Advantages of Combining Traditional Chinese Medicine with Targeted Therapy
Both traditional Chinese medicine and immunotherapy have their respective advantages. In clinical practice, we have observed that combination therapy can yield better outcomes.
1. Higher Efficacy
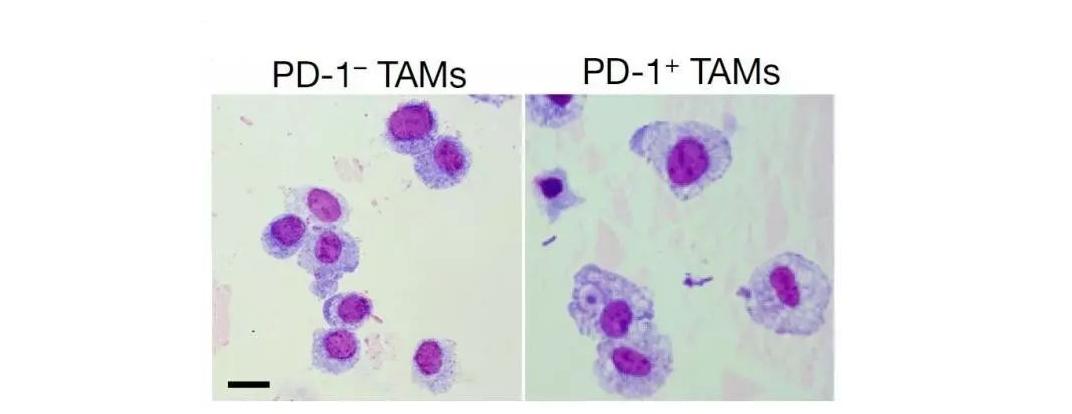
Research from Hebei University of Science and Technology shows that traditional Chinese medicine compounds can interfere with the expression of immune checkpoints PD-1/PD-L1, activate immune helper cells and effector cells, with a principle similar to PD-1 therapy.
The effectiveness of immunotherapy is not very high, and research from Beijing University of Chinese Medicine Dongfang Hospital indicates that after treatment with traditional Chinese medicine, PD-L1 can achieve higher expression. As mentioned earlier, higher expression means higher effectiveness.
2. Reduced Side Effects
One of the advantages of traditional Chinese medicine is its ability to regulate symptoms, whether they arise from the disease itself or from the side effects of medications. Through TCM treatment, patients can experience relief and achieve a better condition to continue their therapy.
3. Delaying the development of drug resistance
According to research from Zhejiang University of Chinese Medicine, the traditional Chinese medicine formula Guilu Erxian Jiao can inhibit tumor proliferation and reverse immune evasion by suppressing the PD-1/PDL-1 signaling pathway. This not only enhances the efficacy of immunotherapy but also delays or even prevents the development of drug resistance.
Drug resistance is a significant cause of tumor recurrence in many patients. The regulation of immunity by traditional Chinese medicine can not only enhance the effectiveness of immunotherapy but also delay the onset of drug resistance, thereby allowing patients to benefit from longer treatment durations and greater therapeutic gains.

4. For Overall Immune Enhancement
Traditional Chinese medicine not only increases resistance to tumors but also enhances overall disease-fighting capabilities. The improvement of overall immunity through traditional Chinese medicine significantly aids in disease treatment and physical recovery.
The combination of traditional Chinese medicine with immunotherapy not only improves the response rate but also alleviates symptoms and side effects, resulting in a better quality of life and prolonged survival.
Research on the combination of traditional Chinese medicine (TCM) with immunotherapy remains limited at present, but it represents one of the future trends. With the advancement of integrated traditional Chinese and Western medicine and the development of immunotherapy, more significant achievements are expected in the field of TCM combined with immunotherapy.
The Future Development of Immunotherapy
Today's immunotherapy is no longer limited to PD-1 and PD-L1; other pathways have also made progress one after another. For example, CTLA-4 inhibitors have already been marketed, and other types of monoclonal antibodies are still under study. In the future, there will be more effective immunotherapy drugs available.
The additional therapeutic effects of the original PD-1 and PD-L1 drugs are also being continuously developed. For example, pembrolizumab, which was initially used for melanoma, has now been applied in the treatment of various malignancies such as non-small cell lung cancer, head and neck squamous cell carcinoma, and classic Hodgkin lymphoma.
Combination immunotherapy is also under continuous investigation. Immunotherapy combined with traditional Chinese medicine, chemotherapy, and radiotherapy has achieved certain results, and the efficacy of combination therapy has also been confirmed. With the advancement of technology, combination therapy will become one of the primary treatment methods in the future.
Conclusion
President Carter's treatment was not solely attributed to immunotherapy. Before taking pembrolizumab, he had undergone comprehensive treatment using various methods. While credit ultimately goes to PD-1, it is also important to recognize the necessity of other treatments. Without surgery and radiotherapy, could tumor control have been achieved solely through pembrolizumab?
Immunotherapy is not 100% effective, and even when effective, it may not necessarily control the tumor. Therefore, while seeking the assistance of immunotherapy, we should not abandon other treatment methods.