Who Decides Whether Cancer Metastasizes? This Test May Be Helpful
Metastasis is one of the characteristics of malignant tumors. Currently, the prediction of malignant tumor metastasis primarily relies on approximate assessments based on disease staging and pathological types. In fact, the accuracy of this evaluation method is not very high. With the advancement of medical testing, many researchers have discovered that circulating tumor cells (CTCs) offer certain advantages in predicting the metastasis of malignant tumors.
I. The Discovery Process of CTCs
In fact, as early as 1869, Australian pathologist Thomas Ashworth discovered during autopsies of patients who had died from malignant tumors that tumor cells from the fatal malignancies were present in the blood vessels of these patients. Based on this finding, he proposed the concept of circulating tumor cells.
However, it was not until the late 1990s that scientists gradually recognized the clinical value of circulating tumor cells. Researchers found that these cells, which detach from primary or metastatic sites and enter the bloodstream due to various reasons during tumor formation or progression, are defined as circulating tumor cells (CTC), abbreviated as CTC.

II. Phenotypes of CTC
CTC exist in various forms in the peripheral blood of tumor patients, including individual free CTCs as well as clustered cell aggregates known as circulating tumor microemboli (CTM).
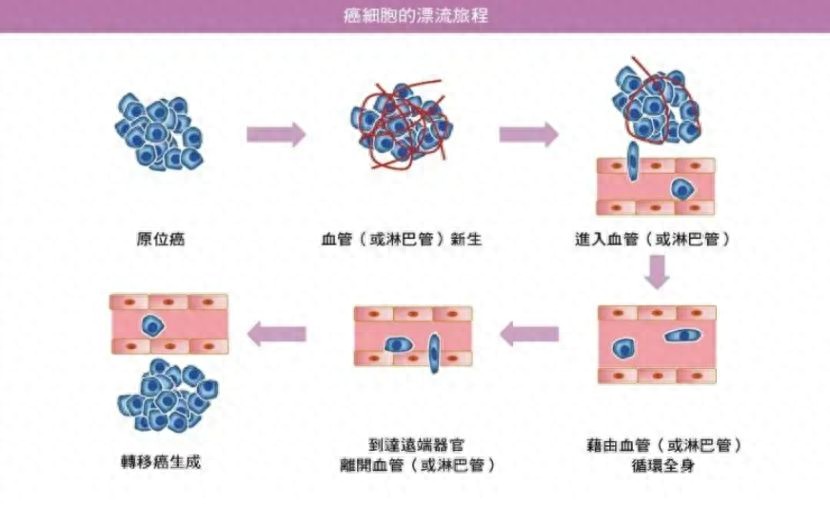
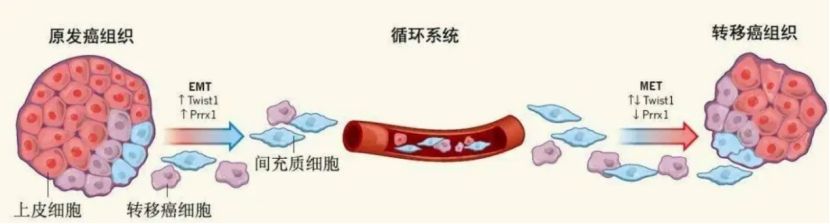
For tumor cells to enter blood vessels, they must traverse the basement membrane. During this process, tumor cells undergo epithelial-mesenchymal transition (EMT), a phenomenon we refer to as EMT.
The occurrence of EMT causes tumor cells to lose epithelial polarity and cell-cell adhesion while gaining invasive and migratory capabilities.
Consequently, when tumor cells enter the peripheral blood to become CTCs, which occurs after the EMT phenomenon, they form three distinct phenotypes: predominantly epithelial tumor cells, predominantly mesenchymal tumor cells, and tumor cells that simultaneously exhibit both epithelial and mesenchymal characteristics.
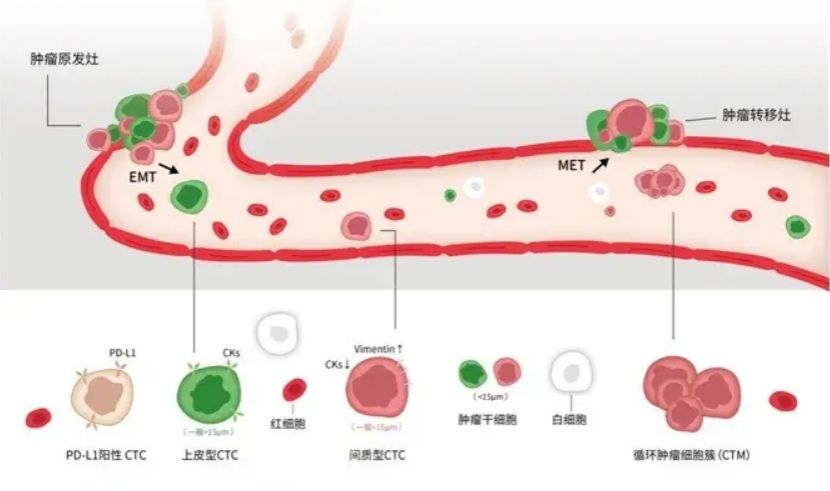
Studies have found that mesenchymal circulating tumor cells exhibit significantly higher malignancy than epithelial or mixed-type circulating tumor cells, enabling them to resist anoikis and tolerate cytotoxic drugs.
If the CTC phenotypic classification detected in the patient's peripheral blood is predominantly mesenchymal-type circulating tumor cells, the risk of tumor recurrence and metastasis in this patient will be significantly increased, indicating a poorer prognosis for the patient.
Therefore, on the basis of CTC counting, further analysis of CTC subtype changes can more comprehensively and accurately assess the risk of tumor recurrence and metastasis in cancer patients.
III. CTC Metastasis
In fact, when CTCs circulate in the bloodstream, most are eliminated due to destruction by shear stress, clearance by the body's immune system, or cellular apoptosis. However, a small portion of CTCs are able to survive and proliferate. It is precisely these surviving CTCs that travel through the bloodstream to target organs and ultimately form metastatic lesions.
Therefore, CTCs are considered an intermediate bridge in tumor metastasis and one of the primary causes of tumor spread.
Additionally, studies suggest that during cancer treatment, CTCs may enter a dormant state and develop some resistance to therapeutic drugs. Once treatment concludes, these CTCs can reawaken and begin proliferating again.
IV. Detection Methods
In recent years, with the advancement of science and technology, an increasing number of scholars have conducted research on CTCs. More new technologies for detecting and analyzing CTCs have been developed, such as novel microfluidic devices, dielectrophoresis, immunomagnetic separation, and in vivo cell collectors. Through these technologies, we can extract CTCs from the peripheral blood of patients with cancers such as breast cancer, hepatocellular carcinoma, prostate cancer, and renal cancer.
V. Significance of Detection
Detecting and analyzing CTC counts in a patient’s peripheral blood holds significant clinical application value. Studies have already established CTC count as a prognostic indicator for various tumors, including breast cancer, prostate cancer, colon cancer, and lung cancer.
CTCs offer advantages over traditional detection methods for screening and diagnosing these cancers and can effectively predict tumor metastasis and prognosis.
Simultaneously, in the treatment of malignant tumors, CTC has been recognized as a novel method for monitoring therapeutic efficacy. When tumors develop drug resistance, the number of CTCs increases over time, and promptly changing the treatment regimen at this stage can minimize ineffective therapy to the greatest extent possible.
Additionally, for advanced cancer patients lacking biopsy conditions, CTC can be used for tumor cell genomic analysis, creating opportunities for targeted therapy or immunotherapy.

Six、Disadvantages
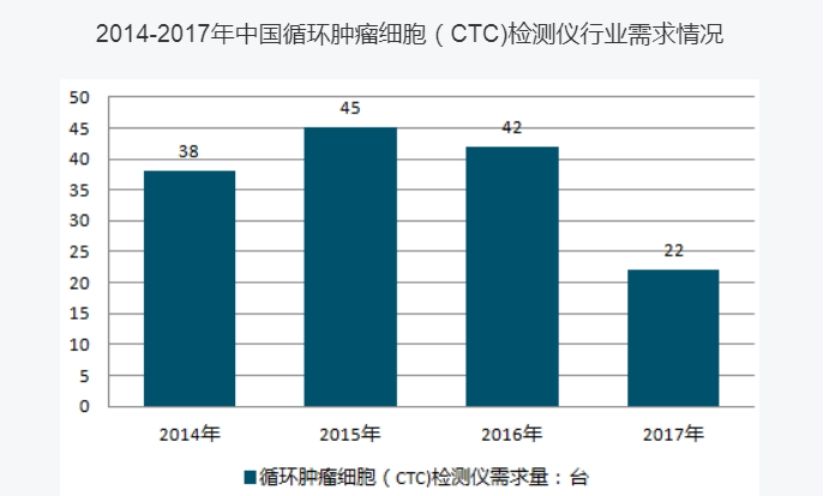
However, CTC testing has not yet been widely adopted in clinical practice. Although it is available in many places, it is currently used by a relatively small population.
Why is this the case?
First, CTC testing is not a traditional diagnostic method, and it will take time for doctors, patients, and the general public to understand and accept this approach.
Second, CTC testing is only a reference diagnostic tool and is not entirely accurate. Both doctors and patients have reservations about whether it is necessary to use this testing method.
Finally, although there are many methods for CTC detection, only one has currently been approved for clinical application, and it is relatively more expensive compared to traditional detection methods.
Although its clinical application is currently limited, CTC detection still holds broad prospects, and scientists are continuously conducting research on it. It is hoped that in the near future, CTC testing will be as widely used in clinical settings as routine blood tests, liver function tests, and kidney function tests.