A 49-Year-Old Woman in Guangdong Went to the Hospital for IUD Removal. When She Woke Up, She Found Herself in the ICU!
To many people, removing an intrauterine device (IUD) is a minor procedure, not even considered a full surgery, often completed in just a few minutes. However, the experience of Ms. Chen (pseudonym), a 49-year-old woman from Guangdong, serves as a heavy warning for all women who may need an IUD removal.
She decided to go to the hospital to have the intrauterine contraceptive device, which had been in place for over twenty years, removed due to lower back pain and discomfort after menopause.
It was supposed to be a simple outpatient procedure, but upon waking from anesthesia, she was shocked to find herself not in the recovery room, but in the intensive care unit (ICU), with tubes inserted into her body and various monitoring devices surrounding her bed.
What happened from the IUD removal room to the ICU?

After emergency treatment and subsequent diagnosis, Ms. Chen had suffered a rare but extremely dangerous complication during the IUD removal procedure: uterine perforation combined with massive hemorrhage and intestinal injury.
Due to years of menopause, her uterus had severely atrophied, the cervical opening was tightly closed, and the originally soft uterine wall had become thin and fragile. Additionally, the IUD had been in place for too long, with parts of it embedded in the uterine muscle layer.
During the procedure, the instrument inadvertently perforated the uterus wall, which was as thin as paper, damaging blood vessels and the adjacent intestine. Massive bleeding and abdominal infection rapidly pushed her to the brink of life-threatening danger.
This extreme case reveals the severely underestimated risks of IUD removal. It is far from a simple "take it out and it's done" procedure. Especially for postmenopausal women, IUD removal is a medical operation that requires serious consideration.

Why Does the Risk of IUD Removal, Especially After Menopause, Increase Sharply?
First Challenge: The "Vast Changes" in the Physiological Structure
After menopause, ovarian function declines and estrogen levels plummet. This directly leads to atrophy of the reproductive system: the uterus shrinks in size, the uterine cavity narrows, and the uterine muscles become thin and lose elasticity; the cervical os atrophies and tightens, sometimes even fusing shut completely.
At this stage, the uterine cavity resembles an old, deteriorating house with contracted internal structures, and the IUD may have already "grown into" the wall (muscle layer embedment).
The doctor operates in a "blind" situation, akin to searching for and retrieving an item embedded in a wall within a narrow, distorted room, where the difficulty and risks are incomparable to those in younger years.

Second Challenge: The "Extended Service" and "Deep Embedding" of the IUD
Intrauterine devices (IUDs) have recommended usage periods, typically ranging from 5 to 15 years.
An IUD that has exceeded its recommended service life may have degraded materials, and more critically, with each menstrual cycle's uterine contractions and the passage of time, the device can become deformed, fractured, or slowly embed into the uterine muscle layer, or even partially penetrate the uterine wall.
In such cases, removing the IUD is no longer a simple "hook and retrieval" procedure but may require "dissection," which carries a high risk of causing uterine perforation.
Third Level: Hidden Diseases "Adding Fuel to the Fire"
Some undiagnosed gynecological conditions, such as endometrial adhesions, large uterine fibroids, or excessive uterine flexion, can significantly complicate and endanger the procedure for IUD removal.
If one proceeds without thorough assessment, it is like navigating through a maze filled with obstacles, where it is easy to "hit a wall" and get injured.

【How to Safely Cross the "Ring Removal" Hurdle? Key Advice for Women】
To avoid the harrowing experience faced by Ms. Chen, postmenopausal women must follow a scientific and rigorous process for ring removal to minimize risks.
1. Timing Selection: Neither too early nor too late is advisable.
The optimal time for IUD removal is within 1 year after menopause, shortly after menstruation has stopped and before the uterus has fully atrophied. At this stage, the cervix remains relatively soft, and there is still some space in the uterine cavity, making the procedure relatively easier. Do not delay until many years after menopause or until your body shows obvious discomfort signals before addressing the issue.
2. Preoperative Assessment: Comprehensive Examination, Do Not Proceed Unprepared
This is the core of safe IUD removal. The following examinations must be performed before the procedure:
Gynecological Ultrasound (including 3D ultrasound if necessary): Accurately determines the position and shape of the IUD within the uterine cavity, checks for embedment or perforation, and assesses the size, endometrium, and myometrium of the uterus.
Cervical Examination: Assess cervical conditions and anticipate the difficulty of dilation.
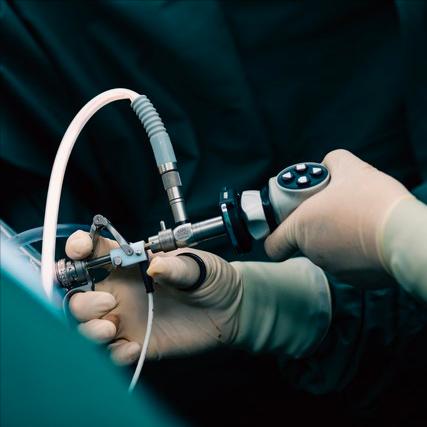
Hysteroscopy as needed: For cases where ultrasound suggests ring embedding, suspected fracture, or intrauterine adhesions, hysteroscopy allows direct visualization and safe removal under direct vision, serving as the gold standard for managing complex situations.
3. Intraoperative preparation: Softening the cervix to create optimal conditions.
For those with atrophic and tightly closed cervix, doctors will administer medications (such as prostaglandin preparations) before the procedure to soften the cervix, making it easier to dilate the cervical os. This can significantly reduce mechanical injury and patient discomfort.
4. Psychological and Medical Preparation: Choose a reputable hospital and trust professional doctors.
It is essential to choose a formal hospital gynecology department with emergency rescue capabilities for the procedure. Fully communicate with the doctor to understand your own condition and surgical risks.
For cases assessed as extremely high risk, doctors may recommend removing the intrauterine device under intravenous anesthesia or even laparoscopic monitoring. This allows for immediate minimally invasive repair in the event of complications such as perforation, avoiding the need for open abdominal surgery.

Mrs. Chen's experience serves as an extreme yet precious warning. It tells us that as the body changes with the passage of time, many "small matters" are no longer simple.
A tiny intrauterine device carries decades of fertility protection, and its safe "retirement" requires equal caution and wisdom on our part.
Menopause is not the endpoint of health but rather the starting point for more meticulous self-management. Facing IUD removal squarely and making thorough preparations is the most responsible attitude toward one's own life and health.