What is the most obvious sign of HPV in women? Doctor: 90% of people ignore it, and if one appears, you should get checked.
Doctor, I don't have any discomfort. How could I be HPV positive? I have increased vaginal discharge and bleeding after intercourse. I thought it was vaginitis, but I didn't expect it to be persistent HPV infection! Every day in the clinic, we encounter such patients. The most cunning aspect of HPV is that in the early stages of infection, there are almost no symptoms. By the time obvious signs appear, it is often already accompanied by cervical lesions. Today, as a gynecologist, I want to clearly tell you:HPV itself has no specific symptoms, but the appearance of these three "abnormal signals" actually indicates that the body is warning that "the virus may have damaged the cervix." Do not mistake them for ordinary inflammation and endure them.。
First, key science: 80% of HPV infections are "transient" and can be cleared by the immune system within 1-2 years, with no symptoms throughout the entire process. Only persistent infection with high-risk HPV for more than 2 years, leading to cervical lesions, will cause noticeable signs. Therefore, these signs are not "infection signals" but "lesion warnings," and prompt screening is essential upon detection.

I. The Most Easily Overlooked Sign 1: Postcoital Bleeding (Non-Menstrual)
This is the most typical sign of HPV-related cervical lesions, yet many people mistake it for "menstrual irregularities" or "cervicitis":
Specific manifestations: After intercourse outside the menstrual period, there may be spotting or blood streaks in the discharge on underwear, with a bright red color, and the amount of bleeding is usually minimal (less than menstrual flow).
Difference from common inflammation: Common cervicitis bleeding is often accompanied by yellow discharge and itching, while bleeding caused by HPV lesions typically presents as "bleeding only, without itching" and recurs repeatedly (occurring during intercourse for 2-3 consecutive times).
Why to be vigilant: Persistent HPV infection makes cervical cells fragile, and friction during intercourse can easily lead to blood vessel rupture. This is an early warning sign of low-grade cervical lesions. If left unchecked, it may progress to high-grade lesions.
Outpatient case: 32-year-old Sister Wang experienced postcoital bleeding for 3 months, initially attributing it to menstrual irregularities. She sought medical examination only after the bleeding increased, and the results showed HPV16 positive + low-grade cervical lesion. Fortunately, it was detected early, and her condition improved through immune system regulation and regular monitoring.
II. Most Easily Confused Sign 2: Abnormal Discharge (Persistent Without Itching)
Many people mistake this discharge for "vaginitis" and use cleansing solutions on their own, only to make the condition worse.
Specific manifestations: Sudden increase in vaginal discharge, appearing as milky white paste-like, rice water-like, or with a foul odor (not fishy odor, as fishy odor is often associated with bacterial vaginosis), persisting for 1-2 weeks without relief.
Difference from common vaginitis: Vaginitis is typically accompanied by noticeable itching and burning pain, with improvement seen within 3-5 days after medication; whereas discharge caused by HPV lesions is characterized by "no itching, no burning pain," simply increased in amount with an odor, and is ineffective against washes and antibiotics.
Why to be vigilant: Cervical lesions can stimulate abnormal secretion from cervical glands. This secretion is a "product" of cell damage. If accompanied by HPV positivity, a colposcopy must be performed for further evaluation.
Three, The Most Easily Misunderstood Sign 3: Cervical Polyps (Small Bumps)
This is a typical sign of low-risk HPV infection, yet many people mistake it for "internal heat" or "inflammatory bumps."
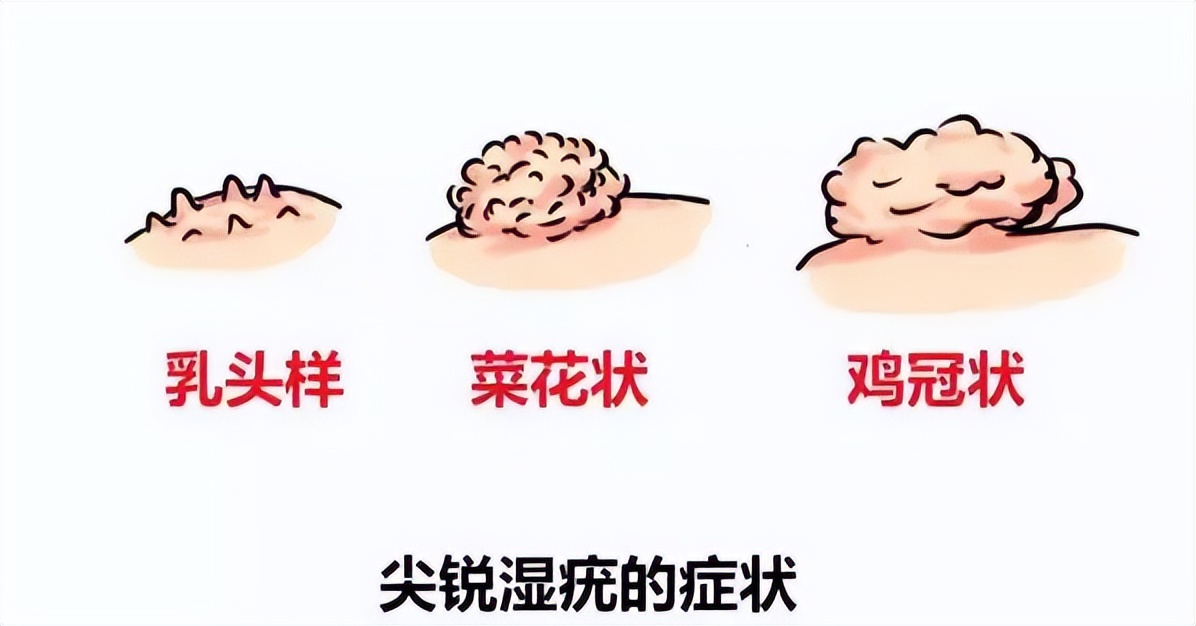
Specific manifestations cauliflower like or papillary small bumps appear on the vulva and cervical opening with a gray white or pink color no pain or itching may be single or multiple clusters
Common Misconception Mistaking it for folliculitis or inflammatory acne and applying ointments without effect
Why to be vigilant: This is condyloma acuminatum caused by low-risk HPV types 6 and 11 infection. Although it is not carcinogenic, it is highly contagious and may be accompanied by high-risk HPV infection. HPV genotyping and TCT must be performed simultaneously.
IV. Core Pitfall Avoidance Guide: These Two Misconceptions Must Be Corrected
1. "No symptoms = No infection" → Wrong!90% of HPV infections are asymptomatic and cannot be determined by "feeling," regular screening is the only method to detect infection.
2. "Having symptoms means it must be cervical cancer" → Wrong!The above signs are mostly manifestations of low-grade cervical lesions or condyloma acuminatum. With timely intervention, 95% of cases can prevent cancer progression, so there is no need for excessive panic.
V. Practical Advice from Doctors: What to Do When Signs Appear
1. Check "HPV+TCT" as soon as possible: Determine whether there is infection with high-risk HPV and whether cervical cells are damaged;
2. If TCT is abnormal or HPV16/18 positive: proceed directly to colposcopy + biopsy to rule out lesions.
3. If diagnosed with condyloma acuminatum: physically remove the warts (laser, cryotherapy), while simultaneously enhancing immunity to prevent recurrence;
4. Regular screening: For ages 21-29, have a TCT every 2 years; after age 30, have HPV+TCT every 1-3 years. Even without symptoms, women who are sexually active must adhere to this.
Finally, I want to say to you:
The most "terrifying" aspect of HPV is not the presence of symptoms, but rather the absence of them—asymptomatic persistent infection is the "silent killer" of cervical cancer. The three aforementioned signs are actually the body's way of "reminding you to stop the damage in time," and should not be mistaken for common inflammation and delayed.
If you are currently experiencing these abnormal signs, do not panic or self-medicate. Go to a regular hospital's gynecology department for screening tomorrow—early detection and early intervention make HPV infection and cervical lesions manageable.