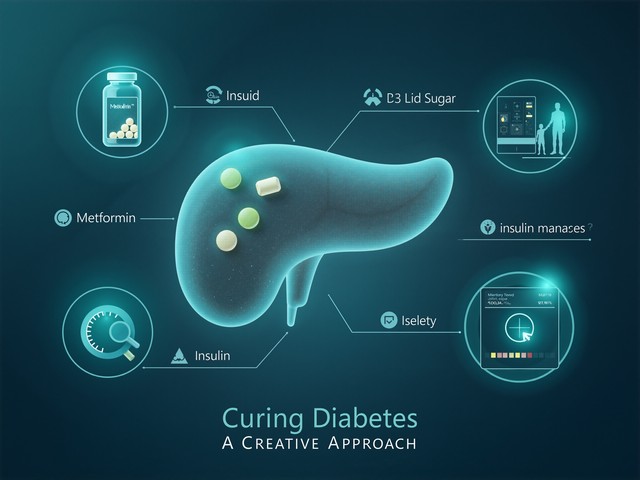
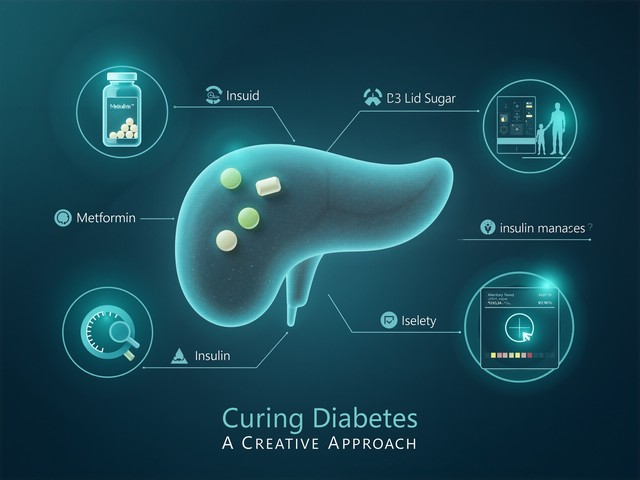
Five types of hypoglycemic drugs: capable of repairing pancreatic islet function
For the vast number of individuals with type 2 diabetes, "lowering blood sugar" is the direct goal of treatment, while hidden behind the fluctuations in blood glucoseDecreased pancreatic islet functionis the core of disease progression. The good news is that the development of modern glucose-lowering drugs has long been not limited to "glucose-lowering" itself.Protect and even to some extent repair the function of pancreatic beta cellshas become an important direction.

Today, let's review several types of glucose-lowering drugs with "pancreas-protective" effects and see how they "reduce the burden" and "provide escort" for your pancreatic islets.
01 Thiazolidinediones: Classic "Insulin Sensitizers"
Representative DrugsRosiglitazone, Pioglitazone.
This class of drugs is known as "insulin sensitizers," which primarily lower blood glucose by increasing insulin sensitivity in skeletal muscle, adipose tissue, and other tissues. Its mechanism of "protecting the pancreas" lies in:
- Reduce the burdenBy improving insulin resistance, the limited insulin in the body can work more efficiently, thereby reducing the pressure on pancreatic beta cells to continuously secrete insulin under high load.
- May promote recoverySome studies suggest that it may have a direct protective effect on pancreatic beta cells, and even some improvement in islet function has been observed in certain patients.
Important NoteBecause it may cause water and sodium retention, increase the risk of heart failure, and potentially affect bone metabolism,Patients with risk of heart failure, severe osteoporosis, or history of fractures should use with caution or avoid.Children, pregnant women, and lactating women are also not suitable for use.
02 GLP-1 Receptor Agonists: The Versatile "Smart Messenger"
Representative drugsLiraglutide, semaglutide, dulaglutide, etc. (including both once-daily and once-weekly dosage forms).
This class of drugs mimics a natural incretin (GLP-1) in the human body, offering comprehensive effects:
- Glucose-dependent insulinotropic secretionIt only works when blood sugar is high, with minimal risk of hypoglycemia.
- Direct protection of beta cellsCanInhibit β-cell apoptosis and potentially promote their proliferation and neogenesisThis is one of its most notable pancreas-protecting properties.
- Comprehensive BenefitIt can also inhibit glucagon secretion, delay gastric emptying, and increase satiety, effectively reducing weight and protecting cardiovascular health while lowering blood sugar.
Important Note:Type 1 diabetes patients are contraindicated.Patients with a personal or family history of medullary thyroid carcinoma or a history of pancreatitis should avoid use. Caution is advised in cases of severe renal impairment.
03 Metformin: New Discovery of "Pancreas Protection" by a Classic Drug
As the first-line and lifelong medication for type 2 diabetes, the pancreatic protective effect of metformin is increasingly recognized:
- Antioxidant and Anti-inflammatoryIt can reduce oxidative stress and inflammatory responses in the body, both of which are important factors that damage pancreatic beta cells.
- Improving Insulin ResistanceAlleviate the secretory burden on beta cells from the source.
Important NoteHigh safety, butSevere renal impairment [eGFR<45ml/(min·1.73m²)] is contraindicatedto prevent the risk of lactic acidosis.
04 Insulin: The Most Direct "Reinforcement" and "Rest Order"
For individuals with diabetes whose pancreatic islet function has significantly declined, exogenous insulin is not only a supplement but also a form of protection:
- Alleviating Glucotoxicity and LipotoxicityRapidly control high blood sugar and eliminate the continuous toxic effects of high glucose and high lipid environments on beta cells.
- Let the islets restThrough exogenous supplementation, the exhausted endogenous beta cells can be granted valuable "rest" time, which may contribute to the partial recovery of their function.
- Improve SensitivityEarly and timely use helps improve insulin resistance in peripheral tissues.
Important NoteDosage requires fine-tuning under medical supervision, with the primary risk beingHypoglycemiaIncreased monitoring is required.
05 Glucokinase Activators: Emerging Stars Targeting the "Blood Glucose Sensor"
Representative DrugsDorzagliatin.
This is a novel oral drug with a new mechanism of action that targets the core glucose-sensing sensor in the human bodyGlucokinase (GK)。
- Repairing the Sensing MechanismBy activating the impaired GK in the liver and pancreas, it restores the body's sensitive perception and autonomous regulation ability to blood glucose changes.
- Source StabilizationTheoretically, it helps to address the issue at its source.Repair the blood glucose homeostasis regulation systemprompting pancreatic beta cells to secrete an appropriate amount of insulin when needed, thereby exerting protective and reparative effects.
Important NoteIt belongs to a relatively new class of drugs, andPregnant women, lactating women, and individuals under 18 years of ageSafety data in this population are insufficient, and its use is currently not recommended.
Expert Reminder
- Pancreatic protection is the outcome of comprehensive managementThe "pancreas-protective" effects of the aforementioned drugs are all established on the basis of effective and stable blood glucose control. Simultaneously,A healthy lifestyle (diet, exercise) is the cornerstone of all treatmentsIt can significantly reduce the burden on the pancreas itself.
- There is no "miracle drug" that can completely reverse it.Currently all medications areIt is impossible to completely prevent the natural decline of pancreatic islet function, let alone thoroughly reverse and restore it.However, they can significantly delay this process and are powerful tools for controlling the condition.
- Individualized selection is the keyEach class of medication has its unique advantages and specific contraindications. The selection of which drug or combination to use must be determined by your doctor based on yourPancreatic function, blood glucose characteristics, body weight, liver and kidney function, cardiovascular status, and personal preferenceComprehensive decision.
- Do not adjust on your own.Please be sure to take medication as prescribed by your doctor. Do not change, add, or stop medication on your own. Regular follow-up examinations, monitoring changes in blood sugar and pancreatic islet function, and maintaining communication with your doctor are the correct ways to achieve long-term stable blood sugar control and protect pancreatic islet function.
Protecting islet function is to win a longer "golden time" for the long-term management of diabetes. Understanding these medications, fully discussing with your doctor, and developing the most suitable individualized plan for you is the most scientific approach to managing diabetes.