Excessive wound drainage after proctological surgery? Don't panic! Follow these care tips to speed up healing by 2x!
Does perianal wound care have you feeling distressed?
Constantly dealing with sticky wound surfaces and persistent drainage, worrying about potential infection; experiencing excruciating pain when dressings adhere to wounds during changes; watching the slow healing progress while fearing scarring might impact daily life..
Actually, most of these anxieties stem from not understanding the "underlying logic" of wound healing! Today, we’ll delve into the core of post-proctological surgery wound care—moist wound healing—to help you avoid pitfalls and literally double your recovery speed.
First, understand: The 4 "challenge stages" of perianal wound healing
The healing of perianal wounds is like building a house—progress happens step by step, with each stage having its own specific "tasks." Effective care depends on finding the right rhythm!
Stage 1: Hemostasis phase (from surgery to a few hours post-op)
Right after surgery, the wound behaves like a "leaky pipe," triggering the body's immediate "emergency response": damaged blood vessels constrict to stop bleeding, while platelets and clotting factors gather to form a "temporary shield." This not only prevents blood loss but also blocks bacterial invasion, laying the groundwork for subsequent healing.
Second Stage: Inflammatory Phase (First 3 Days Post-Surgery)
This is the body's "immune cleanup" phase! Immune cells gather around the wound to clear away necrotic tissue and residual bacteria, making room for new tissue growth. During this stage, some redness, swelling, and mild pain may occur—all of which are normal immune responses.
Stage Three: Proliferation Phase (3 Days - 3 Weeks Postoperative)
This is the "critical construction period" for wound healing! Granulation tissue gradually fills the wound defect, and epithelial cells slowly regenerate, much like "laying new bricks" for the wound. The key during this stage is to provide the granulation tissue with sufficient nutrients and a suitable environment to ensure rapid and healthy growth.
⚫ Phase Four: Remodeling (3+ weeks post-surgery)
The wound is essentially healed and enters the "finishing touches" stage. The newly formed scar tissue further strengthens the wound surface, with complete epithelial coverage, though early-stage scarring may remain noticeable. Proper care can help minimize scar proliferation~
The "secondary healing" shown in the image often aligns with the type of open wounds seen in anorectal surgery.
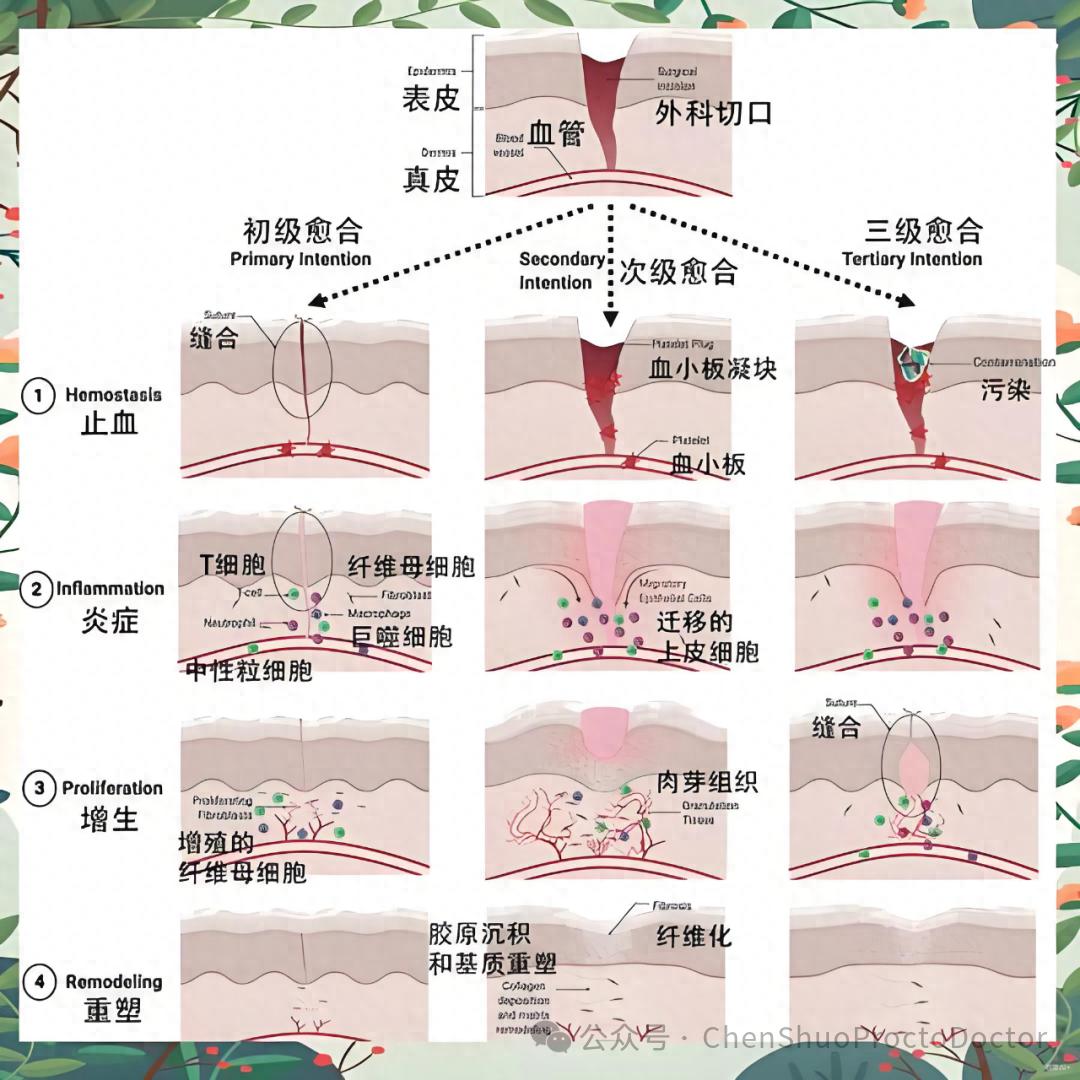
Postoperative anorectal wounds conforming to the "secondary healing" type
Dry Healing vs. Moist Healing: We've Been Getting It Wrong All Along
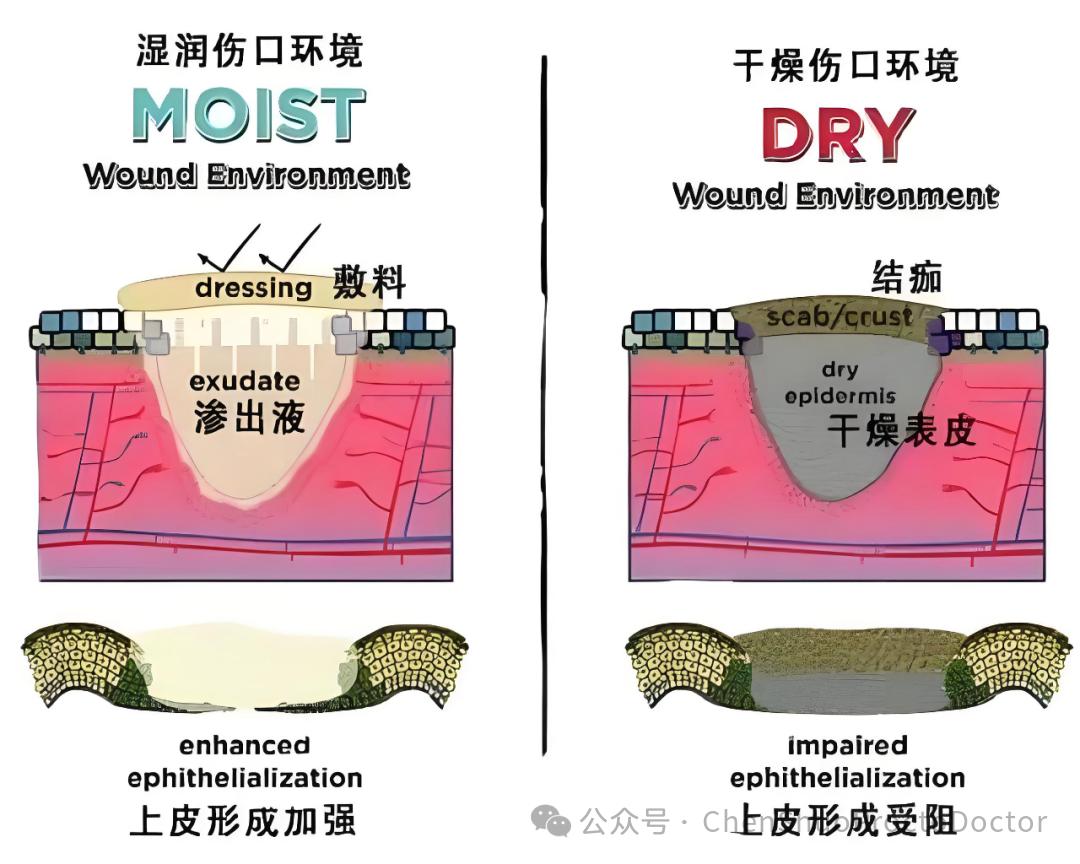
Dry Healing versus Moist Healing
In the past, people believed that "wounds should stay dry and breathable to heal faster" - after all, oxygen promotes healing. However, modern medicine has discovered this notion is actually mistaken!
❌ The 3 Major Drawbacks of Dry Healing
A dry wound is prone to dehydration and scabbing, which acts like "building a wall" for new epithelial cells, hindering their migration and repair;
Dry dressings adhere to the wound, tearing away fragile granulation tissue during dressing changes, essentially "undoing the healing process";
The healing time is prolonged, more visible scars are likely to form, and pain is more intense.
✅ Moist wound healing: Provides "nutrient-rich hydration" to the wound, speeding up healing by 2 times.
The "moist healing" theory proposed by British zoologists has long become the standard care protocol in the medical field, coinciding with the concept of "pus-revitalizing granulation" in traditional Chinese medicine!
Studies confirm that wounds heal twice as fast in moist environments compared to dry ones! The reason is simple:
Wound exudate is not infection, but rather the body's "self-protection" - it contains proteins, amino acids, and cell growth factors, essentially serving as a custom "nutrient solution" for granulation tissue;
A moist environment allows growth factors to function more effectively, stimulating continuous regeneration of granulation tissue
Prevent scab formation and dressing adhesion, reduce pain and tissue damage during dressing changes, and protect the integrity of newly formed tissue.
Key Question: Is persistent wound drainage a sign of infection?
This is the question postoperative patients care about most! The answer is: It’s most likely not an infection, but a normal sign of moist wound healing
To determine if there's an infection, watch for these 2 signs:
Normal exudate: Thick consistency and moderate amount indicate good healing progress (this theory aligns with the traditional Chinese medicine concept of "promoting pus to generate flesh");
Signs of infection: Scarce and thin exudate, accompanied by worsening wound redness, severe pain, fever, etc., requiring immediate medical attention.
Simply put, as long as the exudate has no foul odor and isn't accompanied by abnormal discomfort, let it "flow naturally"—this is your body helping accelerate wound repair~
"Normal exudate": Thick fluid enveloping the wound, indicating granulation tissue growth

Is the "thick discharge" during wound healing a sign of infection?
"Nutritional support activated - healing in progress";
Practical Guide: How to Create a "Moist Healing" Environment?
The key to rapid wound recovery lies in maintaining a moist environment, primarily through two types of "assistants":
1. Ointment / Suppository: The "Moisturizing Protective Film" for Wounds)
Postoperative oily ointments and suppositories for dressing changes! They can form a "protective film" over the wound surface, preventing damage and protecting fragile granulation tissue. Simultaneously, they promote drug absorption through blood circulation, helping the wound expel pus and regenerate tissue, thereby accelerating healing.
2. Moist Dressings: The "Magic Helper" for Healing
Professional moist dressings can precisely maintain wound hydration while also: promoting growth factor release and regulating wound recovery;
They don't adhere to wounds, making dressing changes painless and reducing bleeding;
Protecting nerve endings, reducing pain sensation, and avoiding repeated damage to newly formed tissue.
Final Summary: Key Points of Postoperative Care
Fluid drainage is not scary: it's a normal manifestation of moist wound healing, not infection;
Moisture retention is key: relying on wound exudate + oily ointments + moist dressings to create a "nutrient-rich environment" for granulation tissue;
Avoid common pitfalls: Don't forcibly dry the wound, and don't tear off adhered dressings;
Seek medical attention promptly: If you experience abnormal exudate, severe pain, fever, or other concerning symptoms, be sure to follow up with your doctor immediately.
Most importantly: Dr. Chen Shuo emphasizes that the "moist wound healing" principle mentioned in this article applies only to the wound surface itself. The surrounding healthy skin should remain clean and dry, as failing to do so may lead to eczema-like dermatitis near the wound, causing itching that disrupts sleep and daily life, ultimately hindering proper wound healing.
For postoperative wound care in proctology, finding the right approach helps avoid detours. By following the moist wound healing principle and properly cooperating with dressing changes and care, your wound will heal faster than you imagine!
If you have any questions about postoperative care, feel free to leave a comment below, and let's discuss together. Wishing everyone a speedy recovery!